Thank you to the organisers of the Advanced Technologies and Treatments in Diabetes conference for granting me a press pass to attend this year’s conference virtually. As someone who’s worked in psychosocial health and human factors in technology research, as well as being a user of diabetes technology myself, I couldn’t help but be blown … Continue reading ATTD 2024: How do people REALLY use their diabetes devices?
Author: @T1Bionic ~ Mary Anne Patton
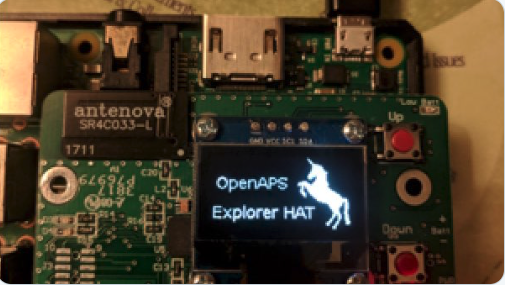
Open source lights the way to better hospital and clinical care in the COVID era
Like most people with diabetes, I’ve been wondering how things would go if I was admitted to hospital with COVID19. I've also been thinking about how patient innovated open source solutions might help diabetes health care providers in this difficult time...
The Joy of Telemedicine
"It's more collaborative, less interrogative." The rise of telemedicine in diabetes has given health care providers a chance to reflect on their practice. What aspects of care can we take forward & improve upon in the post COVID-era? ...
Designing Joy into diabetes apps
When was diabetes ever about joy? How about Fun? Delight? A sense of camaraderie? Everyone needs a pat on the back, a Woo Hoo! and a hand to lift them up when they're feeling down. Reassurance that we're in this together. As humans, we're programmed with a need to belong. But so much of diabetes care, … Continue reading Designing Joy into diabetes apps
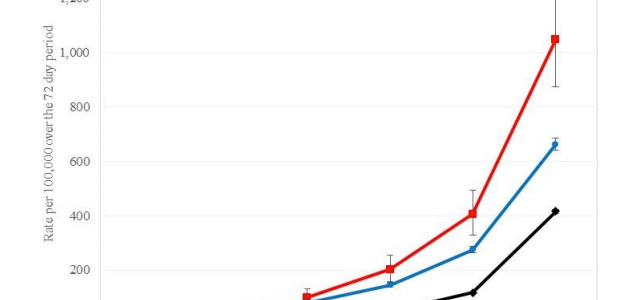
COVID-19: Today’s diabetes therapy is tomorrow’s outcome data
Reading through the latest COVID-19 diabetes statistics from the UK/NHS , I'm reminded that I'm in a much stronger position today with my blood glucose levels than I was two years ago. Thanks to DIYAPS. I'm not about to kid myself that I'm invincible - far from it - But it's sobering to realise that if I … Continue reading COVID-19: Today’s diabetes therapy is tomorrow’s outcome data
Ypsomed partners with Dexcom, promises future closed loop using TypeZero algorithm
Medtronic paradigm (522) & Ypsomed Ypsomed and Dexcom have just announced their partnership (4 May 2020) and say a future version of the Ypsomed pump will loop with the TypeZero algorithm, the algorithm used in Tandem's ControlIQ. This partnership is a step forward for a company that says it is committed to patient choice and … Continue reading Ypsomed partners with Dexcom, promises future closed loop using TypeZero algorithm
Ben West – fixing diabetes, changing the conversation
It’s hard to write about Ben West without “feeling it deep in the heart” as Weston Nordgren put it so well on Twitter. I've been fascinated by Ben ever since I discovered the lengths he went to to liberate diabetes data over a five year period, starting in 2009. Ben's work, Decocare, formed the central part … Continue reading Ben West – fixing diabetes, changing the conversation
My diabetic sister & Dr Montgomery
I sometimes wonder how life would have turned out if Julie really was my diabetic sister. Maybe I never would have thrown the baby out with the bath water? Maybe I never would have felt the need to make the pact? Life turned out pretty well anyway, but it could have been so much easier. For all of … Continue reading My diabetic sister & Dr Montgomery
Ruby
Ruby was five, in overalls and fairy wings, legs swinging fast beneath the chair that was too high for her. "Would it be ok for Ruby to touch your Dexcom?" her father asked. "Sure," I said, and shimmied over to where Ruby was sitting. She reached over and traced the Dexcom bump through my sleeve. I asked her … Continue reading Ruby
The wave of sadness – unexpected
When I switched on my OpenAPS 'artificial pancreas' in May 2018, it was the end of a long wait. A 38 year dream come true. I bounced around like a maniac for months on a high, and my gratitude to the smart, kind people who developed the system knew no bounds. What I wasn't prepared … Continue reading The wave of sadness – unexpected