First published in Australian Diabetes Educator, 8 July, 2019.
Patton, Mary Anne. “One year of DIY looping after 38 years of type 1 diabetes.” Australian Diabetes Educator, vol. 22, no. 2, 2019.
Introduction
One year ago I started do-it-yourself (DIY) looping with the hybrid closed loop system, OpenAPS.[1] I’d been living with type 1 diabetes (T1D) for 38 years and had dreamt of a closed loop solution since I was diagnosed at 12 years of age.[2]
The impact of this technology on my life has been so profound, both physically and psychologically, that it feels as though I am no longer even dealing with the same medical condition. I now have access to ‘high fidelity therapy’ [3], and I am thrilled that commercial products are beginning to roll into the market so that, provided we get funding systems in place to ensure access, all people with T1D could soon have an opportunity to reap the benefits that people in the DIY community have been able to experience.[4-9]
In this article I aim to show how great the impact of hybrid closed looping has been for me, and to outline the features of OpenAPS and Nightscout [10] that have stood out for me as being particularly beneficial. Note that people with diabetes have found all three DIY systems (AndroidAPS, Loop and OpenAPS) to be extremely effective, and each system has its own advantages.[1, 11-13]
Glycaemic impact
As for most people [14] my main motivation for using a DIY system was to improve glycaemic control by automating it. The results were immediate and dramatic.
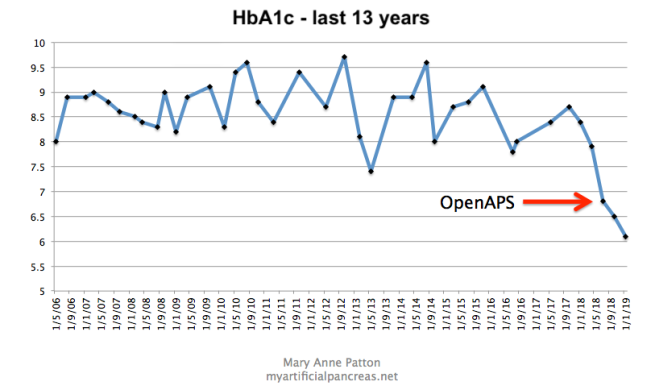
- Figure 1. HbA1c over the last 13 years
I’d made many attempts to stabilise my diabetes and reduce my HbA1c over the years, but unfortunately, pre-looping, when my blood glucose levels (BGLs) were in the normal range I often felt hypoglycaemic, or as though I was about to have a hypo. This ‘living on the edge of a hypo’ feeling led me to subconsciously develop strategies, such as under-bolusing for meals, in order to avoid hypoglycaemia. In hindsight I think continuous glucose monitoring (CGM) may have helped with this – I relied on manual blood glucose monitoring until two months before starting OpenAPS – but there were many features of OpenAPS and Nightscout that provided the real key.
I needed a system I could learn to trust over time that would minimise my glycaemic variability, help me to avoid hypoglycaemia, and put me firmly in the driver’s seat.
Adjusting to a new sense of normal
The OpenAPS algorithm, by adjusting insulin delivery through setting temporary basal rates, based on CGM readings every five minutes, automatically reduced my BGLs towards the target I’d set. I initially set my target to around 6.5mmol/L while I was getting used to the system and the lower levels, but within weeks I had reduced my target to 5.5mmol/L.
The ambulatory glucose profile (AGP) from Dexcom Clarity over this first year of looping shows this BG normalisation process and the reduction in glycaemic variability over time.
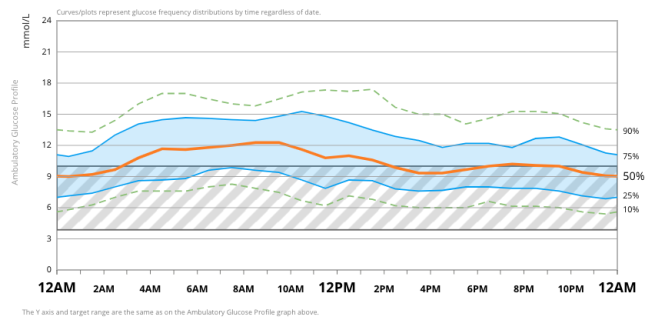
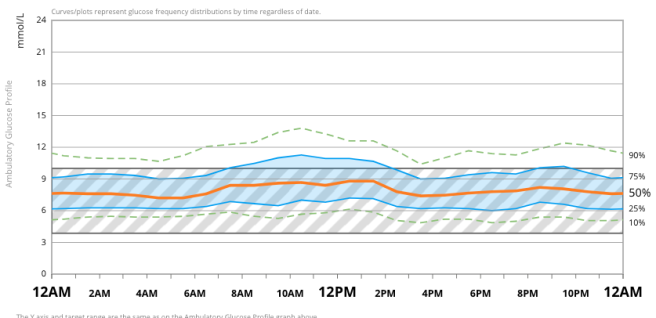
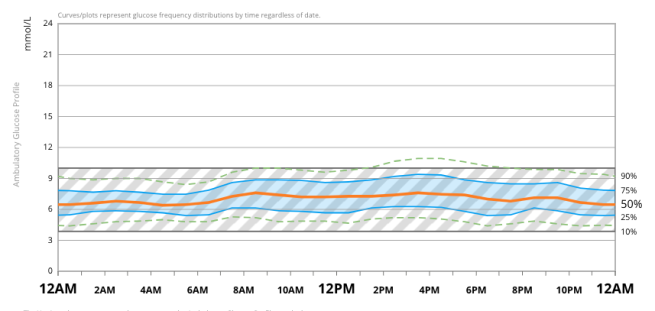
I learned to customise my settings during this time and to adjust them ‘on the fly’ to achieve the results I wanted.[15] Trust in the system developed quickly. Real time data visualisation through the Nightscout website meant I had the confidence to adjust my diabetes behaviours (such as bolus and hypo treatment behaviours) based on feedback I was getting from the system. Over time, the positive feedback loop of OpenAPS and Nightscout visualisation enabled me to readjust to what ‘normal’ levels felt like as I developed a new blood glucose homeostasis.
Realtime data visualisation
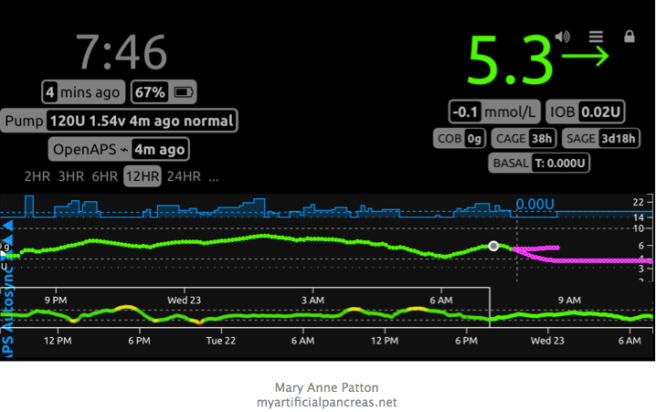
Being able to see my detailed data on my mobile phone, at a glance, any time, and to be able to interact with it ‘on the fly’ was exactly what I needed. Mostly I just glance at the CGM glucose line to see what my glucose level is doing (green), the basal line (blue) to see how much insulin I’ve got on board, and the prediction lines (purple) to see what’s likely to happen next. But I can also see how many carbs I’ve got on board, when I last changed my insulin pump site, when I last changed my CGM sensor, how much battery charge is left in my pump and in the Edison/Explorer board rig that runs the system, and how much the glucose levels are deviating from what was expected. I can change the view to a two hour, three hour, six hour, twelve hour or 24 hour view, and I can run reports on predicted HbA1c, average sensor glucose, time in range, standard deviation and more, with just a couple of clicks.
I can’t overemphasise how valuable it was to be able to see this information in real time during my first year of looping, and how much it contrasted to the old way of doing things – downloading BG test results and pump data, using proprietary systems retrospectively, with a lot of effort.
In addition to what I can see at a glance about what is happening in the moment, I can run reports from my mobile phone or computer any time, to check my predicted HbA1c, time in range, average glucose and glucose variability. Most importantly, I can interact with the system quickly and easily to get it to behave differently.
Am I about to have a hypo?
Here is one example of a typical circumstance in which the OpenAPS/Nightscout combination has been critical for establishing trust and changing behaviour.
I loved the Dexcom display, and CGM was a major step forward from finger-prick BG monitoring alone, but as someone concerned about ‘living on the edge of a hypo,’ this type of visual feedback would likely have sent me reaching for glucose.

Compare that to what I was able visualise through Nightscout using OpenAPS just a few moments later.
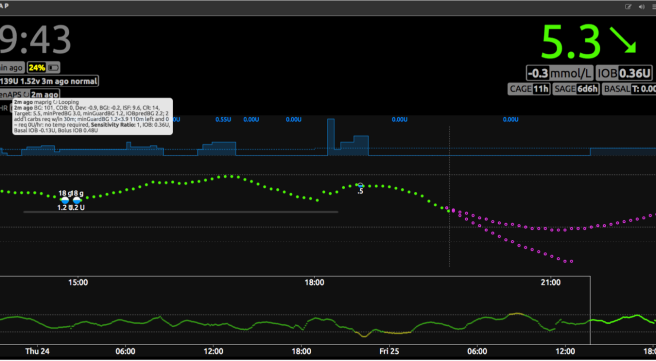
I could see from the basal line (figure 7) that I had had no insulin delivered for the previous hour and a half because OpenAPS had suspended the insulin due to predicting a low BG. I can also see from the prediction lines that my BG is expected to level off at, or just below, 4mmol/L. If I click on the OpenAPS pill, I can see that the system is recommending I consume 2 grams of carbohydrate in the next 30 minutes to remain in my BG target range. Many people using OpenAPS have this ‘carbs required’ information sent to them automatically as a notification.
Not only is this reassuring, but it gives me options. If I am about to drive, or have a work deadline, for instance, I will choose to eat carbohydrate. If I’m at home relaxing I might just wait it out and see what happens because I have the reassurance from the system that my BGs are not likely to drop too low. Note that with hybrid closed loop systems only a small amount of carbohydrate is generally needed to correct lows because the system has already been suspending insulin.
Autotune
One brilliant feature of OpenAPS is Autotune. It is a program that runs automatically every night and iteratively calculates insulin sensitivity factor (correction factor), basal rates and carb to insulin ratio, based on real data, and uses these values in the next day’s predictions. Most people find testing settings difficult, particularly basal testing, so this program is extremely helpful.
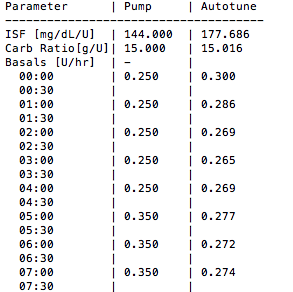
Autotune enabled me to discover that I was much more insulin sensitive than I realised. It turned out that one unit of insulin dropped my glucose level by almost 10mmol/L. This sensitivity, along with my pre-looping glycaemic variability (standard deviation pre-looping was 3.6mmol/L, post-looping it is around 1.8mmol/L) gave me insight into why I’d often felt on the verge of hypoglycaemia prior to looping. If my BG was 5.5mmol/L it really could drop to 2.5mmol/L very quickly. And the under-bolusing behaviour I’d developed for meals also made sense to me now that I realised how insulin sensitive I was. Overestimating the amount of carbohydrate in a meal, and bolusing for it, could lead to severe hypoglycaemia.
Meal bolusing
A number of options for meal bolusing with DIY systems exist.[16]
The fact that OpenAPS allowed separation of carbohydrate announcement and bolusing for meals was incredibly helpful for me. Prior to looping I had used the normal bolus, dual wave or square wave bolus functions of my pump, for example giving a three-unit bolus with one unit up front and the rest over a one-hour period. Given that three units would drop my blood glucose by around 30mmol/L, a miscalculation (overestimate) of carbs could easily lead to hypoglycaemia, and so I often subconsciously under-bolused.
I was now able to tell the system how many carbohydrates I was about to eat, but I only needed to bolus for part of it. I had a system using a dynamic carbohydrate absorption algorithm to sort out the rest of the insulin via temporary basal rates, based on how rapidly my blood glucose was rising or falling after a meal. This reduced my tendency to under-bolus, and increased my carb counting accuracy, as I no longer had the fear of bolus-induced hypoglycaemia.
Note that most people use the super micro bolus advanced feature of OpenAPS for meals [17] but I do not have this feature enabled due to my high insulin sensitivity. I either bolus from my pump bolus wizard or, for slow absorbing meals, sometimes just use a carbohydrate announcement through iPhone shortcuts.[15]
Unannounced Meals
An advanced feature of OpenAPS that I enabled after the first month of using the system is Unannounced Meals. This gives the algorithm the power to detect when I have underestimated carbohydrates, based on blood glucose deviations, and give more insulin accordingly.
Autosens
Another excellent advanced feature I have enabled is Autosens. This detects and responds to sensitivity changes that are caused, for example, by hormones, pump site changes, sick days and stress. Like all features of OpenAPS there are safety caps which constrain how much OpenAPS can adjust settings, but it helps keep BGs in range by modifying basal rates, insulin sensitivity factor and temporary BG targets.
Ease of use
Good usability of diabetes devices is absolutely critical for quality of life with diabetes. I love that I can interact with the system ‘on the fly’ either through the Nightscout site or through the iPhone shortcuts that I’ve set up.[15]
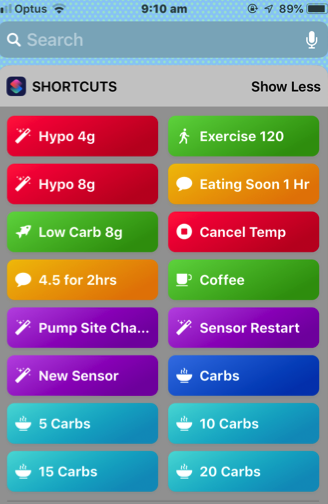
With only a swipe and a click or two I can tell the system how many carbs I’m about to eat, that I’ve changed my pump site or sensor, or set a temporary BG target. The ‘eating soon’ button gets the system to aim for a BG of 4.5mmol/L for one hour, which gets the insulin going before meals, helps control post meal spikes, and can be a safer option for many people than pre-bolusing.
A reassuring shortcut is the hypo recovery shortcut. It tells the system I’ve had 4 or 8 grams of carbohydrates and also tells it to raise my BG target for the next half hour to allow me to recover from the hypo.
Note, some people have set up ‘Hey Siri’ or ‘Ok Google’ voice commands as an alternative to interact with their systems and once again, each DIY system will have different options for this type of control.
Conclusion
Every morning when I wake up to a BG of 5.5mmol/L or close to it, I am reminded of how grateful I am to have access to looping technology. I am extremely grateful to the pioneers who created these systems and shared them openly via open source software. [3, 18-24] I am also extremely grateful to the people testing and enhancing these systems, and the people supporting this vibrant community. The years of dedication involved are staggering to contemplate. Finally, I am grateful to my partner, who has IT expertise, for setting OpenAPS up for me.
I share my story to convey just how powerful this type of technology can be. The three DIY systems in use in Australia are all highly effective.[5] AndroidAPS, which uses the OpenAPS algorithm, can be used with brand new in-warranty pumps.[13, 24] US-based non-profit, Tidepool [25], has initiated a project to build and support an FDA-regulated version of the DIY system, Loop, and has a vision to partner with a range of commercially available insulin pump companies. Commercial off-the-shelf solutions are emerging[24]. But there is no point in having the technology if people can’t afford it. I believe this technology holds the key to putting an end to T1D complications. Now is the time for us to ensure that funding and subsidies are in place so that all people with T1D can benefit.
(You can hear more about the very personal impact of DIY looping for me and Jim Matheson, one of the first 16 loopers in the world, on ABC Science Show’s podcast. DIY ‘loopers’ take diabetes into their own hands.)
References
- 2017. Available from: https://openaps.readthedocs.io/en/latest/
- Patton, M. My Artificial Pancreas. 2017 Nov. Available from: https://myartificialpancreas.net/
- West, B. No tools exist to audit medical devices. 2012 June 20. [Updated 2018 Nov 12] Available from: https://github.com/bewest/insulaudit/issues/1
- Crabtree T, McLay A, Wilmot E. DIY artificial pancreas systems: here to stay? Practical Diabetes. 2019 Mar;36(2):63-8.
- Hng TM, Burren D. Appearance of Do‐It‐Yourself closed‐loop systems to manage type 1 diabetes. Internal medicine journal. 2018 Nov;48(11):1400-4.
- Lewis D, Leibrand S, # OpenAPS Community. Real-world use of open source artificial pancreas systems. Journal of diabetes science and technology. 2016 Nov;10(6)
- Lewis D, Swain R, Doneer T. Improvements in A1C and time-in-range in DIY closed-loop (OpenAPS) users.
- Litchman M, Lewis D, Kelly L, Gee P. Twitter analysis of# OpenAPS DIY artificial pancreas technology use suggests improved A1C and quality of life. Journal of diabetes science and technology. 2019 Mar;13(2):164-70.
- Petruzelkova L, Soupal J, Plasova V, Jiranova P, Neuman V, Plachy L, Pruhova S, Sumnik Z, Obermannova B. Excellent Glycemic Control Maintained by Open-Source Hybrid Closed-Loop AndroidAPS During and After Sustained Physical Activity. Diabetes technology & therapeutics. 2018 Oct 25;20(11):744-50.
- The Nightscout Project | We Are Not Waiting. Cited 2019 Apr 28. Available from: http://www.nightscout.info/
- DiSimone, Loop Tips. K. Available from: https://kdisimone.github.io/looptips/
- Loop Docs. Available from: https://loopkit.github.io/loopdocs/
- Welcome to the AndroidAPS documentation. Available from: https://androidaps.readthedocs.io/en/latest/EN/
- DIWHY Braune K, O’Donnell S, Cleal B, Willaing I, Tappe A, Lewis D, Hauck B, Scibilia R, Rowley E, Ko W, Doyle G. DIWHY–Motivations, barriers and retention factors of DIY artificial pancreas users in real world use: The BolusCal2 Study, an open-label, randomized controlled trial. In Advanced Technologies & Treatments for Diabetes 2019 (Vol. 21, No. S1).
- Patton, M. iPhone shortcuts for OpenAPS. 2019 Jan 8. Available from: https://myartificialpancreas.net/2019/01/08/iphone-shortcuts-for-openaps/
- Street, T. Meal times when closed looping: some points to consider. Diabet-tech Diabetes and Technology. 2019 Jan 25. Available from: https://www.diabettech.com/artificial-pancreas/ meal-times-when-closed-looping-some-points-to-consider/
- Street, T. Understanding SMB and oref1. Diabet-tech Diabetes and Technology. 2019 Feb 14. Available from: https://www.diabettech.com/artificial-pancreas/understanding-smb-and-oref1/
- Gottlieb, S. The FDA, Patient Empowerment, and the Type 1 Diabetes Communities in the Era of Digital Health. Platypus. The CASTAC Blog. 2019 Apr 23. Available from: http://blog.castac.org/2019/04/the-fda-patient-empowerment-and-the-type-1-diabetes-communities-in-the-era-of-digital-health/
- Gottlieb, S. and Cluck, J. Going Rogue: Re-coding Resistance with Type 1 Diabetes (In press) Digital Culture and Society.
- Kresge, N and Cortez, M. The $250 biohack that’s revolutionizing life with diabetes. Business Week. Bloomberg. 2018 Nov 6. Available at: https://www.bloomberg.com/news/features/2018-08-08/the-250-biohack-that-s-revolutionizing-life-with-diabetes
- Lewis D. History and perspective on DIY closed looping. Journal of Diabetes Science and Technology. 2018 Oct 22:1932296818808307.
- Racklyeft, N. The history of Loop and Loopkit. Medium. 2016 Oct 13. Available from: https://medium.com/@loudnate/the-history-of-loop-and-loopkit-59b3caf13805
- Schwamb, P. Insulin Pumps, Decapped chips and Software Defined Radios. Medium. 2019 Apr 25. Available from: https://blog.usejournal.com/insulin-pumps-decapped-chips-and-software-defined-radios-1be50f121d05
- Burren, D. Closed loop pumps in Australia. 2019. Available from: https://bionicwookiee.com/closed-loop-pumps-in-australia/
- Tidepool Loop. Available from: https://www.tidepool.org/loop
Thanks for taking time to share your experience with DIY looping. What platforms do you share your other amazing insite?
LikeLike
Hi Bobbie. Thanks for that great feedback. I’m on Twitter @T1Bionic and on YouTube as My Artificial Pancreas. I’ve been interviewed on ABC Science Show. If you have suggestions on other platforms that would enjoy my articles I’d love to hear about them.
LikeLike